Acute Calculous Cholecystitis
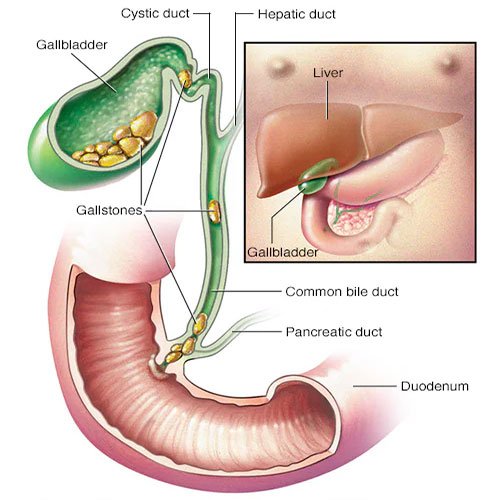
Acute calculous cholecystitis is an inflammation of the gallbladder due to the presence of gallstones, which obstruct the cystic duct. This condition is characterized by sudden onset of abdominal pain, usually in the right upper quadrant, and may be accompanied by nausea, vomiting, fever, and leukocytosis. It is a common surgical emergency and can lead to serious complications, including perforation of the gallbladder, peritonitis, and sepsis if not treated promptly.
The primary cause of acute calculous cholecystitis is gallstones, which are hardened deposits of digestive fluid that can form in the gallbladder. When a stone lodges in the cystic duct, it can cause increased pressure within the gallbladder, leading to ischemia and inflammation. Risk factors for developing gallstones include obesity, pregnancy, certain diets (high in fat and cholesterol), and genetic predisposition.
Symptoms
- Severe pain in the right upper abdomen or epigastric region, often radiating to the right shoulder or back
- Nausea and vomiting
- Fever and chills
- Tenderness in the right upper quadrant
- Murphy’s sign (pain upon palpation of the gallbladder during inhalation)
Diagnosis: Diagnosis is typically made based on clinical history, physical examination, and imaging studies. Ultrasound is the first-line imaging modality and can show gallstones, thickening of the gallbladder wall, and pericholecystic fluid. A CT scan may also be used for further evaluation.
Treatment
Initial Management:
- Supportive Care: Intravenous fluids, electrolyte management, and analgesics to control pain.
- Antibiotics: Broad-spectrum antibiotics are initiated to cover potential infections, particularly if there is concern for perforation or other complications.
Surgical Treatment:
- Cholecystectomy: The definitive treatment for acute calculous cholecystitis is the surgical removal of the gallbladder (cholecystectomy). This can be performed laparoscopically or through an open approach, depending on the severity of the condition and the patient’s overall health. Laparoscopic cholecystectomy is preferred due to its minimally invasive nature, reduced recovery time, and lower complication rates.
- Timing of Surgery: Traditionally, surgery was performed within 48 to 72 hours of diagnosis to reduce complications. Recent studies suggest that early cholecystectomy (within 24 hours of admission) is safe and may improve outcomes.





